Understanding Disruptive Behavior Disorders in Children
Disruptive behavior disorders (DBDs) may be to blame when a child’s behavior becomes unmanageable. Parents and caregivers should be aware of the signs and symptoms associated with DBDs so they can identify them early on and seek out help. This article will explore the different types of DBDs and how they can affect a child’s daily life.
Disruptive behavior disorders (DBD) can have a detrimental effect on the life of a child. Such behaviors are characterized by disobeying authority figures and displaying inappropriate responses to them, ranging from unsympathetic indifference to strained hostility. It is not just the individual that suffers; those around them can also feel the aftereffects of living with someone affected by DBD. The most common types of this disorder are ODD, CD, and unspecified or other disruptive behavior disorders. Children facing these issues often demonstrate intense feelings of annoyance and frustration while being obstinate, disobedient, and quarrelsome toward people in positions of power.
What are Disruptive Behavior Disorders?
Disruptive behavior disorders (DBDs) are a type of mental health disorder characterized by ongoing patterns of uncooperative and defiant behavior. These types of behaviors tend to negatively impact the day-to-day life of those affected by them and those around them. DBDs are most commonly seen in children, although adults can also experience them. Several different types of DBDs can occur in children, including oppositional defiant disorder (ODD), conduct disorder (CD), and intermittent explosive disorder (IED).
Symptoms of disruptive behavior disorders can vary depending on the specific disorder, but some common signs may indicate a child has a problem. One of the most common disruptive behavior disorder symptoms is acting out in school. This may include behaviors such as talking back to teachers, getting into physical altercations with other students, or disrupting class with constant movement or noise. Another common symptom of a disruptive behavior disorder is difficulty following rules at home and in other settings. This may manifest as defiance of authority figures, refusing to do chores or homework, or engaging in risky or destructive behaviors.
Children with disruptive behavior disorders often have trouble making and keeping friends. They may be aggressive or bullying towards others, which can lead to social isolation. Disruptive behavior disorders can also cause problems in a child’s academic performance. They may have difficulty paying attention in class, struggle to complete assignments or receive lower grades than they are capable of earning. Many children with disruptive behavior disorders also exhibit signs of impulsivity and hyperactivity. They may be constantly on the go, have trouble sitting still, and be impulsive in their actions and decisions.
Some children with disruptive behavior disorders may also have difficulty regulating their emotions. They may seem angry or irritable much of the time and have outbursts of anger that are disproportionate to the situation.
Disruptive behavior disorders can also cause sleep problems in children. They may have difficulty falling asleep or staying asleep through the night, leading to fatigue during the day. Appetite changes are another common symptom of disruptive behavior disorders. Children may lose interest in food or become picky eaters, leading to weight loss or poor nutrition.
Children with the oppositional defiant disorder often lose their temper. They are quick to argue with adults over rules or requests.
Children with oppositional defiant disorder (ODD) can be difficult to manage due to their frequent outbursts of bad temper. They usually take a confrontational attitude towards adults, often refusing any rules or requests established for them. These episodes of resistance can lead to feelings of frustration and powerlessness in both the child and the adult trying to help. ODD can have serious implications on the quality of life for everyone involved, so it is important that children exhibiting signs of this disorder receive prompt attention from mental health professionals who can provide parents with an intervention plan.
They are likely to:
Be uncooperative
Oppositional defiant disorder (ODD) is a behavioral disorder that presents in children and predisposes them to be uncooperative and defiant. This could include constant arguing with adults, refusing to obey rules, purposely annoying people, and being easily annoyed by others. ODD typically develops in children between the ages of two and three. Although ODD can present differently among individuals, it often persists until adulthood if not addressed. Parents need to seek immediate professional help if they feel their child has ODD so that it can be managed early on.
Argue, even about small and unimportant things.
Children with the oppositional defiant disorder (ODD) often engage in argumentative behavior, which can go beyond simple disagreements. ODD is characterized by a persistent pattern of angry outbursts, argumentativeness, and defiance towards authority figures that can start as young as preschool age and usually continue until adulthood. Not only are children with ODD more likely to argue with authority, but they will also argue even when the topic isn’t critical, or there is no clear point to be made. They may also claim for an excessively long duration rather than dropping the subject, making them challenging to appease or resolve conflicts. Parents of children suffering from ODD should seek therapeutic techniques that are proven effective to help them better manage their emotions and have more productive conversations with their children.
Refuse to follow the rules.
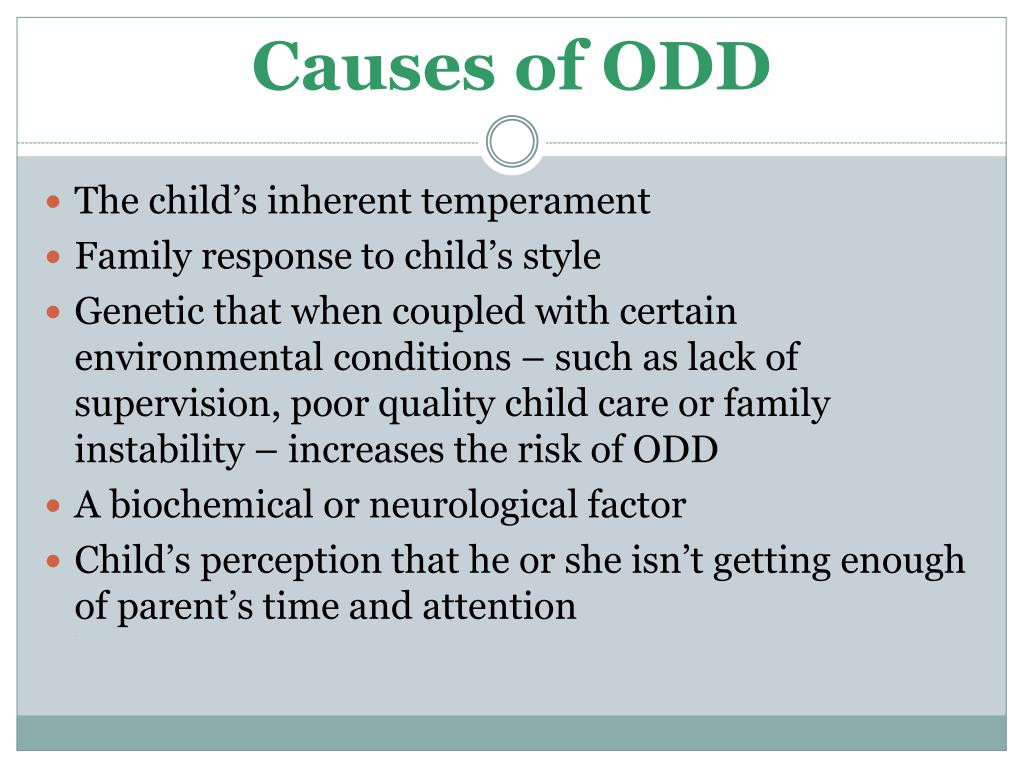
Oppositional defiant disorder (ODD) is a common behavioral disorder in children. ODD presents as extreme defiance, rebelliousness, aggression, and a solid refusal to follow the rules and comply with authority figures. More than occasional outbursts, ODD involves an ongoing pattern of disruptive and disobedient behavior that disrupts an individual’s home, school, and social life. The root causes of ODD are often complex and might include a combination of genetics, environment, psychological factors, or even physiological influences. Regardless of its origin, it is essential to recognize the patterns associated with ODD so that the necessary steps can be taken for appropriate diagnosis and treatment.
Deliberately annoy others, and become easily irritated by other people.
Children with the oppositional defiant disorder (ODD) often display rebellious and disobedient behavior to annoy others purposely. This could include talking back, purposefully disobeying rules and commands, argumentative, and being deliberately irritable. On the flip side, ODD kids also tend to be easily annoyed by other people – this could manifest in sensitivity to criticism or feeling overwhelmed when given direction from teachers or parents. As a result of their diagnosis, loved ones need to understand this condition and show empathy as they help these children learn to manage their emotions.
Blame others for their mistakes or misbehavior.
Children with oppositional defiant disorder often blame others for their mistakes or misbehavior. This tendency results from some children’s difficulty taking responsibility for their behavior and the emotional distress caused by the disorder. They may not acknowledge that they did anything wrong and instead point fingers at peers, teachers, family members, or even strangers to place the blame onto someone else. The best way to help a child who exhibits this behavior is through patient support, understanding, and guidance into more productive coping methods such as deep breathing, journaling thoughts and feelings, or other activities that can increase emotional regulation. With help from adults, children with the oppositional defiant disorder can learn healthier ways to handle difficult experiences.
Behave in angry, resentful, spiteful, and vindictive ways.
Children with oppositional defiant disorder (ODD) often display a consistent pattern of behaviors demonstrating a lack of compliance or hostility towards authority figures. ODD is typically seen in children ages 2 to 8, whose behaviors range from arguing, outbursts, and non-responsiveness, to physical aggression and refusal to follow the rules or regulations. Unfortunately, these angry and resentful responses usually result in negative consequences; parents must seek professional help to manage the challenging behaviors associated with this disorder. The earlier ODD is addressed, the more successful treatment efforts will likely be. With appropriate interventions like psychotherapy and family counseling, it is possible to help a child learn how to appropriately express their thoughts and emotions in ways that do not involve aggression or a vindictive attitude.

Common Symptoms
Children who suffer from a disruptive behavior disorder often display certain behaviors that are considered to be outside the norm for their age group or development level. Common symptoms include frequent outbursts or temper tantrums, aggression towards peers or family members, difficulty following rules, refusal to comply with requests or instructions, and difficulty controlling emotions or impulses. It is important to note that these symptoms may vary depending on the specific type of DBD being experienced by the child.
Disruptive behavior disorders such as Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD) affect millions worldwide, yet their exact causes are still poorly understood. It is believed that multiple pathways can lead to these disorders developing, those being a combination of biological and environmental influences. For example, genetics may play a role in the likelihood of a person developing a disorder; however, research suggests that the environment also affects how symptoms manifest over time.
Factors such as poor parenting styles, lack of consistent disciplinary strategies, or other family dysfunctions can create an environment where younger members are more likely to develop a disruptive behavior disorder. In addition, psychological factors such as inadequate self-esteem or difficulty managing emotions can make it difficult for children who already possess these traits to develop effective coping mechanisms or take responsibility for their actions. By uncovering these various contributing factors, it may be possible to start providing effective interventions and treatments to those affected by these conditions.
Heredity. Children with disruptive behavior disorders often have parents with mental health disorders, including
Substance abuse.
Substance abuse has proven to be a significant contributor to Disruptive Behavior Disorders (DBDs). Alcohol and other drugs can reduce self-control, impair judgment, and increase aggression, which supports the idea that substance addiction can cause DBDs. Various studies have confirmed that individuals with a history of substance use are more likely to have disruptive behaviors detracting from their everyday functioning. Additionally, the range of abuse types and frequency needed to increase the chances of developing extreme changes in behavior differs depending on the individual. While it is not commonly thought of as such, addiction should be considered a form of mental disorder.
Attention-deficit/hyperactivity disorder.
Attention-deficit/hyperactivity disorder (ADHD), a hyperkinetic disorder, is a mental health disorder characterized by difficulty concentrating, impulsivity, and being easily distracted. These symptoms can lead to disruptive behavior disorders such as oppositional defiant disorder (ODD) and conduct disorder (CD). ODD is a pattern of hostile and disobedient behavior commonly involving problem behaviors such as defiance, verbal aggression, and refusal to follow instructions. CD occurs when children engage in conduct that violates the rights of others or significant societal norms. It includes aggressive behavior toward people or animals and destructive, manipulative, and deceitful behavior. Most individuals with ADHD have at least one other comorbid condition, including conduct/oppositional defiant disorder, anxiety disorders, sleeping disorders, or learning disabilities. Understanding the role of ADHD in influencing coordination deficits can help caregivers create strategies for managing disruptive behaviors within the home environment.
A mood disorder.
A mood disorder is a mental health condition that can cause severe emotional shifts. Individuals experience extreme sadness, emptiness, lack of motivation, and difficulty controlling their emotions. Studies have shown that this intense emotional state can persist for weeks or months and manifest into physical symptoms, such as headaches and dizziness. When these feelings last for an extended period, they can cause individuals to engage in disruptive behavior disorders like Attention Deficit Hyperactivity Disorder (ADHD). ADHD has been linked to depression and low self-esteem since it lowers productivity and concentration levels. Unfortunately, disruption caused by the disorder can result in strained relationships between family, friends, and coworkers due to difficulty communicating while feeling overwhelmed by events around them. It is important to remember that mood disorders are not easily managed without proper medical attention; it is essential to access professional help if you feel any signs of these symptoms.
Schizophrenia.
Schizophrenia is a severe mental health condition characterized by changes in perception, thinking, and behavior, and can lead to Disruptive Behavior Disorders. It occurs when individuals experience symptoms of hallucinations and delusions, which often involve false beliefs about the world around them. Disruptive Behavior Disorders are marked by impulse control or hyperactivity difficulties, which can disrupt mood, communication, and socialization. Common signs of schizophrenia include difficulty concentrating, problems making decisions, sleeping difficulties, and trouble initiating activities or conversations. Treatment typically includes psychiatric medications and psychotherapy to assist patients in managing the behavioral issues associated with their disorder. Through early diagnosis, medication management, and ongoing support from friends and family members- those who have schizophrenia have the potential to live productive lives.
Antisocial personality disorder.
Antisocial personality disorder (ASPD) is a psychological condition that can lead to behavior problems, including eating disorders, disruptive behaviors, and impulsive activities. It is estimated that up to 3% of men and 1% of women suffer from this disorder in adulthood. Individuals may have difficulty regulating their emotions and are inclined to reckless or selfish behaviors. Furthermore, individuals may become irritable when things don’t go their way and break rules by lying or becoming aggressive in certain situations. Disruptive Behavior Disorders often manifest due to the symptoms of ASPD as there are limited problem-solving skills to manage uncomfortable feelings or confusion. Unsurprisingly, these behaviors interfere with social relationships and can even lead to legal consequences. Awareness of mental health difficulties such as ASPD is paramount if we will support those struggling with this condition long-term.

Treatment Options
It is possible for children with DBDs to lead successful lives with proper treatment and support from family members and professionals alike. Treatment options for disruptive behavior disorders may include individual or family therapy, medication management, social skills training, parent education programs, academic support services, and other behavioral interventions such as positive reinforcement strategies or cognitive behavioral therapy (CBT). Working closely with your doctor to find an effective treatment plan that works best for your child’s needs is essential.
Disruptive behavior disorders can seriously impact a child’s daily life if left untreated. Early diagnosis is key in helping children manage their symptoms effectively to lead successful lives despite their diagnosis. Suppose you suspect your child may be suffering from a disruptive behavior disorder. In that case, it is important to speak with your doctor immediately to determine the best course of action for treatment and support. With a proper understanding of these conditions and proper intervention strategies in place, it is possible for children with DBDs to live happy and fulfilling lives!
Contact us today at 816.819.5166 or schedule your appointment online.